The Evolution of Remote Patient Monitoring in Clinical Trials
Remote patient monitoring (RPM) has come a long way from the early days of paper-based symptom diaries and intermittent in-clinic assessments. Traditional monitoring approaches placed a heavy burden on both patients and research sites, requiring frequent visits, manual data entry, and limited insight into patient health between appointments. These methods often resulted in gaps in data, delayed responses to adverse events, and high dropout rates.
Today, RPM has transformed into a sophisticated, data-driven component of decentralized clinical trials. Thanks to advances in wearable technology and digital health tools, researchers can now collect continuous, real-time data directly from participants regardless of their geographic location. Devices like smartwatches, biosensors, and mobile health apps have opened the door to remote monitoring that’s not just more convenient, but also more accurate and comprehensive.
Behind the scenes, cloud-based platforms and artificial intelligence (AI) are streamlining the aggregation and analysis of these large data sets. With AI, study teams can spot trends early, respond to safety signals faster, and make more informed decisions about trial progression—all while minimizing patient burden.
As RPM evolves, its integration with machine learning, predictive analytics, and user-friendly interfaces will continue to reshape how trials are designed, executed, and experienced.
Benefits of Remote Patient Monitoring in Decentralized Clinical Trials
RPM isn’t just a convenience; it’s a catalyst for making clinical trials more efficient, inclusive, and patient-friendly. As decentralized trials continue to gain traction, the value of RPM becomes increasingly clear across several dimensions.
Real-Time Data Collection
RPM devices enable continuous health monitoring, generating rich, real-time datasets. This immediate access to patient data improves accuracy and allows researchers to detect potential safety concerns or efficacy trends early (sometimes even before symptoms emerge). AI-enhanced analytics can sift through these massive datasets quickly, delivering actionable insights without overwhelming site staff.
Improved Patient Compliance and Engagement
By reducing the need for frequent in-person site visits, wearable devices lower the burden of participation for patients. This is especially beneficial for populations who may struggle with travel, such as the elderly or those in rural areas. Patients are more likely to stay engaged and complete the study when participation feels less intrusive. Tools like ePRO and eCOA also make it easier for participants to report outcomes from home, boosting both compliance and data quality.
Lower Trial Costs
Automated data collection reduces reliance on manual processes and minimizes the need for site infrastructure and staffing. These operational efficiencies can significantly lower trial costs, especially in large, geographically dispersed studies.
Diversity and Inclusion
RPM broadens trial access by reaching patients beyond traditional site boundaries. This helps include underrepresented groups, improving the generalizability of trial results and supporting equity in research.
Integration with Predictive Analytics
When paired with predictive modeling, RPM doesn’t just show what’s happening now—it can forecast what might happen next. This proactive insight allows sponsors to make data-driven adjustments mid-study, improving outcomes and resource allocation.
Together, these benefits underscore why RPM is fast becoming a cornerstone of modern clinical trial design.
The Future of Wearable Devices for Remote Patient Monitoring
Wearable technology is rapidly evolving, and its impact on RPM in decentralized clinical trials is only beginning to be realized. From biosensors to implantables, the next generation of devices promises to deliver richer data, greater accuracy, and more seamless integration into patients’ everyday lives, transforming how trials are conducted and monitored.
Next-Generation Biosensors
Today’s biosensors can already monitor vital signs like heart rate, blood pressure, and respiratory rate. But the future points to devices capable of continuously tracking a wider range of biomarkers such as hydration levels, oxygen saturation, and even mood indicators, through compact, skin-adhering sensors. These will not only collect data passively but also provide real-time alerts when intervention is needed. Paired with AI, these sensors can help detect anomalies before they become problems, enhancing safety and responsiveness.
Smartwatches and Fitness Trackers for Clinical Research
Smartwatches have moved far beyond step counts. In the clinical setting, they now track metrics like heart rate variability, oxygen saturation, and sleep cycles. As more of these consumer-grade devices become FDA-cleared, they are poised to become valuable tools for collecting reliable clinical-grade data at scale. Their widespread adoption and user familiarity also make onboarding patients smoother and faster.
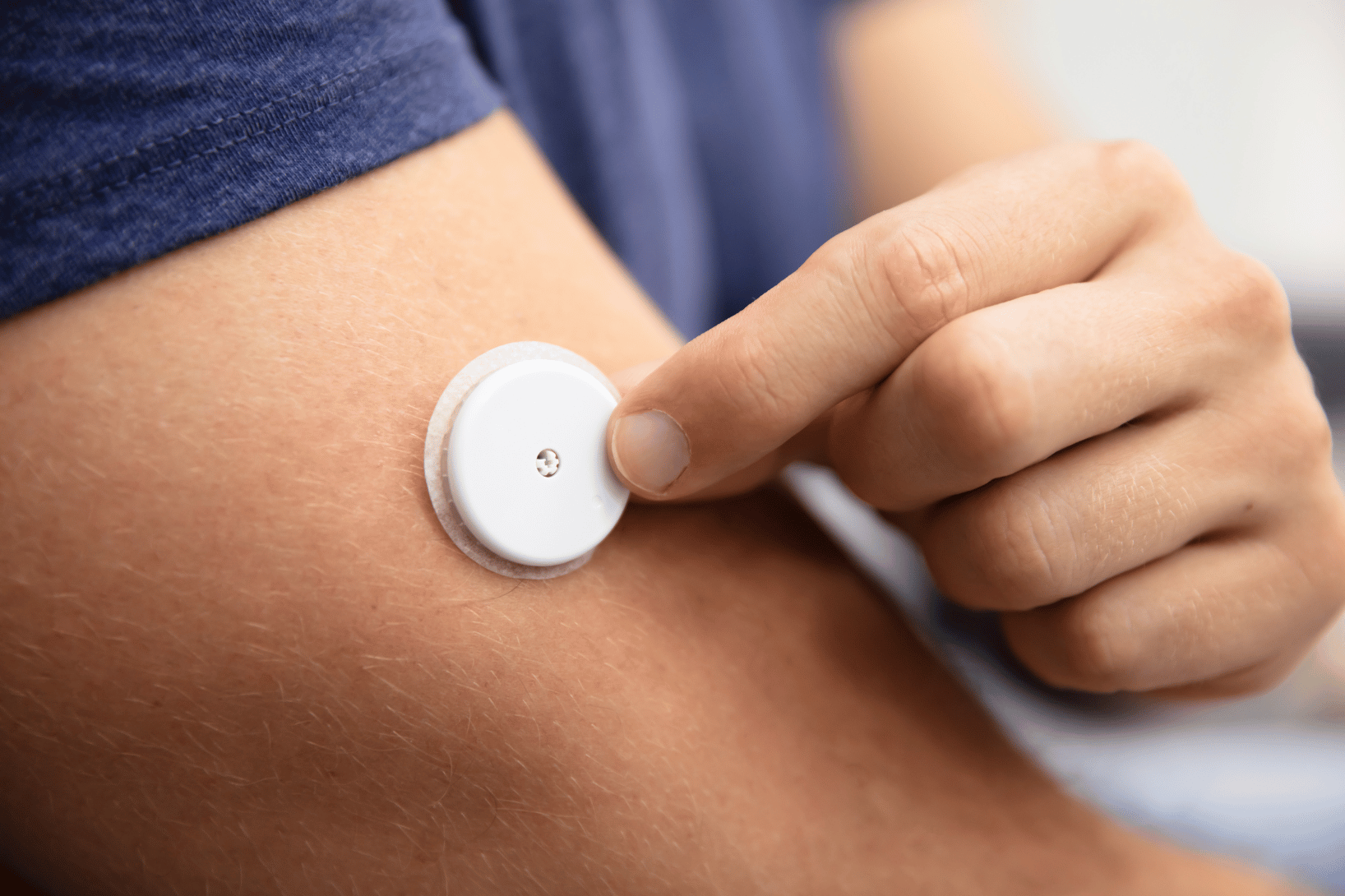
Continuous Glucose Monitors and Metabolic Wearables
RPM is especially impactful in chronic disease trials. Continuous glucose monitors (CGMs) are now essential in diabetes research, allowing for real-time blood sugar tracking without finger sticks. Looking ahead, metabolic wearables that measure multiple biomarkers such as insulin, ketone levels, and cortisol could bring a more holistic view of a patient’s health, enabling personalized interventions and more targeted therapies.
Implantable and Long-Term Monitoring Devices
Minimally invasive implantables offer continuous data capture for extended periods, making them ideal for long-term safety and efficacy studies. These devices can monitor heart rhythms, neurological activity, or medication adherence with precision, and AI-driven data processing will further enhance their utility. As these tools become more refined and less obtrusive, we can expect greater adoption in trials that require high-resolution longitudinal data.
AI and Data Analytics: The Force Multiplier
The future of RPM hinges not only on the devices themselves but also on how their data is used. AI and machine learning will continue to automate data cleaning, flag anomalies, and enable predictive health insights. These capabilities will help researchers move from reactive to proactive decision-making, enabling earlier interventions, fewer protocol deviations, and better patient outcomes.
Wearables are no longer just accessories—they’re evolving into essential, intelligent instruments that are reshaping clinical trial conduct from the ground up.
Regulatory and Compliance Considerations for the Future of RPM
As RPM becomes more integral to decentralized clinical trials, staying aligned with evolving regulatory expectations is critical. Agencies like the FDA and EMA are actively shaping guidance for the use of digital health technologies, emphasizing the importance of data integrity, device validation, and patient safety.
Data privacy is also top of mind. With sensitive health information flowing through cloud platforms and wearable devices, trial sponsors must ensure compliance with HIPAA, GDPR, and other data protection laws. Technologies like blockchain and advanced encryption are gaining traction as tools to safeguard patient data and build trust.
Digital consent forms are simplifying compliance, making it easier for participants to understand and authorize data collection and monitoring remotely.
Looking ahead, achieving standardization and interoperability across devices and platforms will be key to realizing the full potential of RPM while keeping patient rights and safety front and center.
Overcoming Challenges in Remote Patient Monitoring
RPM isn’t without its hurdles. For RPM to truly support decentralized clinical trials at scale, sponsors and CROs must overcome several persistent challenges, from ensuring device accuracy to managing the avalanche of data that comes with continuous monitoring.
Data accuracy starts at the device level. Not all wearables are created equal. Clinical-grade sensors must be validated and regularly calibrated to avoid misleading or incomplete data. AI can help flag inconsistencies, but garbage in still means garbage out. Choosing the right technology partners—and holding them to rigorous standards—is essential.
Patient engagement is another linchpin. Even the most advanced tech is useless if patients don’t use it properly. That’s where tools like virtual visits come in. A well-timed telehealth call can answer questions, resolve confusion, and rebuild trust when patients feel overwhelmed by devices or apps.
And then there’s the data—huge volumes of it. Without the right infrastructure, teams risk drowning in information with no way to extract insight. That’s why flexible, unified platforms are critical. With the right technology backbone, teams can not only manage the scale of RPM data but make it actionable.
This is where TrialKit stands out. As a powerful, unified platform, TrialKit gives sponsors and researchers the ability to integrate everything—telehealth, eCOA, wearable data, and more—into a secure, centralized environment. Whether you’re running a hybrid study or a fully decentralized trial, TrialKit brings order to complexity and turns data into decisions.
RPM is changing the landscape of clinical trials, but only if we’re bold enough to tackle the challenges head-on with the right tools in hand.
FAQs About Remote Patient Monitoring in Decentralized Clinical Trials
What Is Remote Patient Monitoring in Clinical Trials?
Remote patient monitoring (RPM) uses wearable devices and digital tools to collect real-time health data from participants outside traditional clinic settings. It enables continuous monitoring without requiring frequent in-person visits.
How Is Artificial Intelligence Changing Remote Patient Monitoring?
AI automates data analysis, detects early warning signs, and supports real-time decision-making. It reduces manual work while improving data accuracy and responsiveness in clinical trials.
What Are the Future Trends in Remote Patient Monitoring?
Expect more advanced biosensors, implantable devices, multi-biomarker tracking, and seamless AI integration. Fully virtual trials and enhanced data security measures will also become more common.
How Secure Is Remote Patient Monitoring Data?
Data privacy is protected through HIPAA- and GDPR-compliant systems. Encryption and emerging tools like blockchain enhance security and transparency in digital health data management.
Will Remote Patient Monitoring Replace Traditional Clinical Trials?
Not entirely. RPM will complement (not replace) traditional models, enabling more hybrid and decentralized trial designs that offer flexibility while preserving scientific rigor.